We’re excited to share the recent publication of important work led by the Adult Genetics Unit and the Cancer Statewide Clinical Network within the CEIH. Published in the Asia-Pacific Journal of Clinical Oncology, this research describes the development, implementation, and evaluation of a statewide mainstream genetic testing model designed to improve access and enhance cancer treatment decision making.
Why is germline genetic testing important?
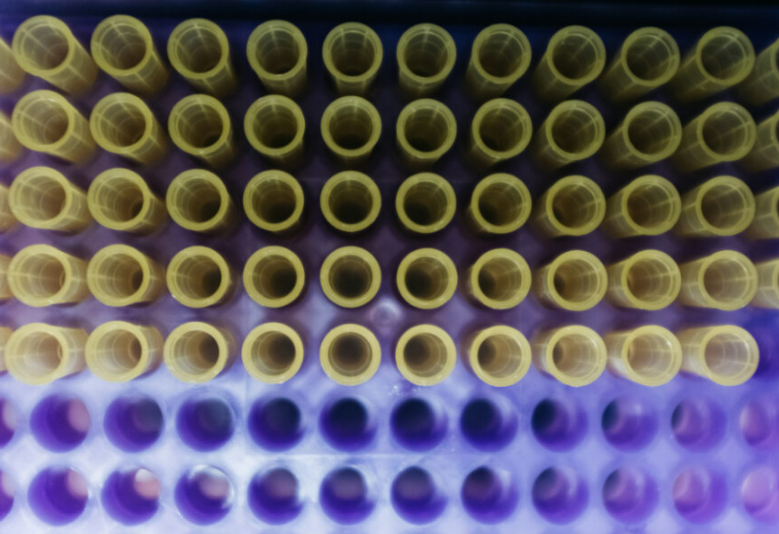
Germline genetic testing identifies inherited gene changes that can significantly influence cancer risk, diagnosis, and treatment. Early and widespread access to these tests enables tailored patient care, informs treatment options, and helps guide family risk assessments — all vital components of precision oncology and effective cancer control.
The project aimed to create a streamlined and consistent pathway that supports patients accessing germline testing. Guided by implementation science and a collaborative approach, the team worked closely with clinicians, genetic specialists and consumers to develop practical tools, education programs, and workflow-aligned pathways. This model covers multiple cancer types and spans metropolitan and regional health networks, fostering equity and efficiency across diverse clinical settings.
Key outcomes include:
- A substantial increase in BRCA1/2 genetic tests ordered through the mainstream pathway, reflecting improved access.
- High levels of clinician and patient acceptability of the mainstream testing model.
- Valuable insights into implementation challenges for Mismatch Repair (MMR) gene variant testing (related to Lynch Syndrome), highlighting the need for tailored approaches.
- Identification of barriers such as time pressures and data monitoring difficulties, with ongoing partnership and responsive strategies critical to overcoming these.
This project utilised the CEIH Project Lifecycle, which is freely available on our website. The framework integrates implementation science and research-to-action principles throughout stages of the project – from initial planning and design to evaluation and ongoing improvement. By following the Project Lifecycle, the team maintained strong stakeholders engagement, incorporated real-world feedback, and adapted the program as needed. This practical, structured approach supports effective improvements in the health system and enhances the translation of research into routine clinical practice.
The CEIH team looks forward to sharing more about this project at the upcoming Evidence and Implementation Summit, showcasing how integrating a statewide project lifecycle with a research-to-action framework supports meaningful change in cancer care pathways.
We extend sincere thanks to SA Pathology for their vital contribution in enabling high-level data oversight to evaluate and monitor germline testing rates. We also acknowledge the Cancer SCN and its sub-working group for their expertise and dedication, as well as all clinicians, patients, and stakeholders who provided input throughout the project.
Want to learn more about this initiative, visit our project page here:
Statewide Framework for Cancer Care Germline Testing