Dr Phil Worley, Clinical Lead for the Statewide Surgical and Perioperative Care Clinical Network and Consultant General Surgeon, provides an update on a major body of work for 2022.
The Statewide Surgical and Perioperative Care Clinical Network has been investigating how we can best deliver Optimised Surgical Care to all patients undergoing a surgical procedure across South Australia, including an in-depth research review.
Despite recent advances in surgical and anaesthetic techniques, poorly prepared patients are at increased risk for major perioperative complications and longer hospital stays. A review of research clearly demonstrated that poor health and functional fitness has an impact on post-operative outcomes and quality of life.
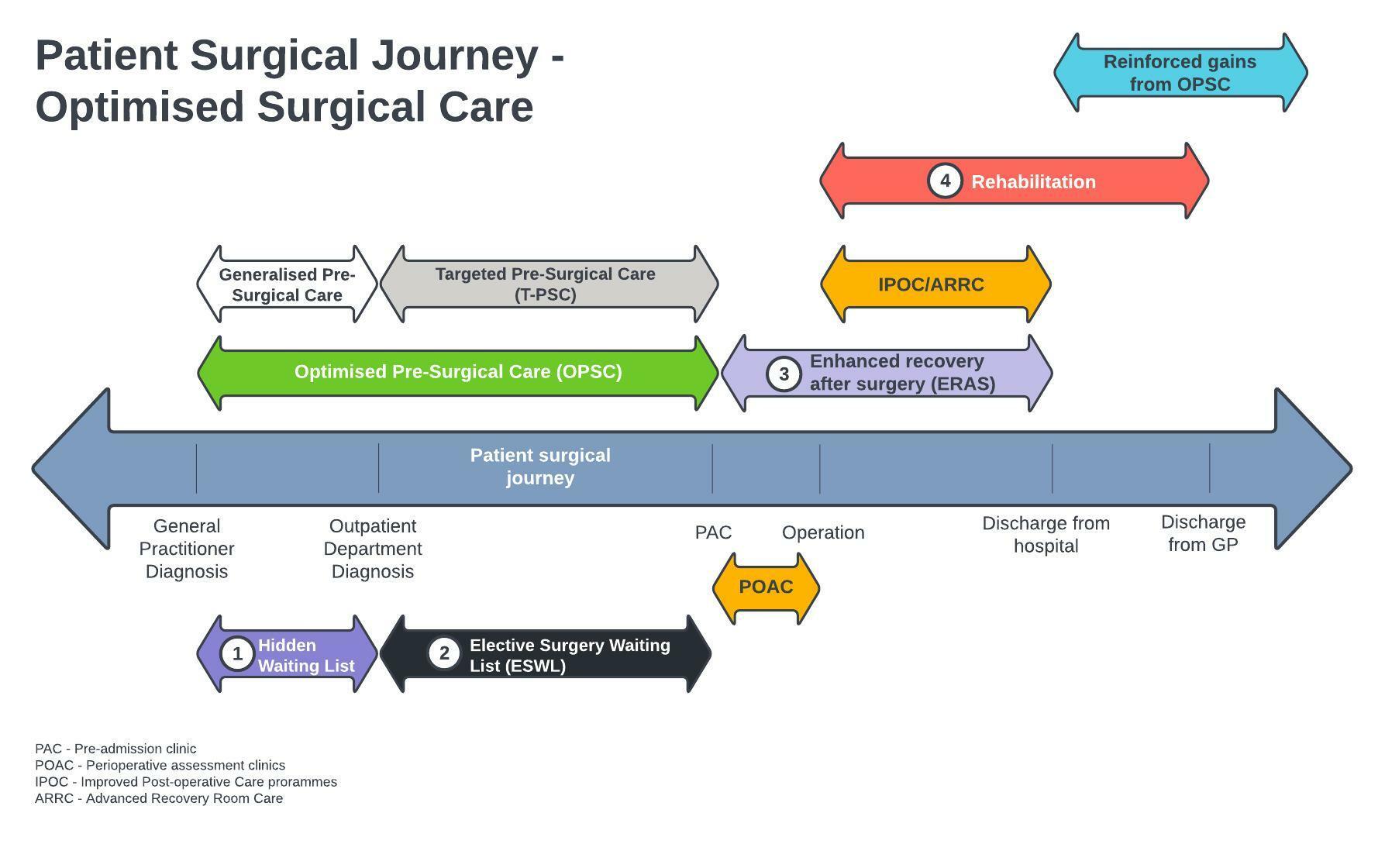
If we were to look at a patient’s surgical journey, from the time that their General Practitioner (GP) refers them to a specialist outpatient clinic, through to them being discharged from the specialist’s care back to the GP, we could divide this time into four main periods:
- The time from GP diagnosis, and referral to the specialist, until the patient is first seen by the specialist (hidden surgical waiting list)
- The time from when the specialist and patient decide that a surgical procedure is required, up until when the patient is seen in the Pre-Admission Clinic (Elective surgical waiting list — ESWL)
- The time from being seen in Pre-admission to being discharged from hospital (Peri-operative period)
- The time from surgery to discharge back to the GP’s care (Post-operative care)
In South Australia we have good services in place for minimising the ‘peri-operative’ risks, usually commencing from the time a patient is seen in the pre-admission clinic. However, there is often only a very short time prior to their actual surgery, and this may inhibit any chance of more significant interventions to optimise the patient’s condition prior to their procedure. We are left with ‘doing the best we can’ with the patient’s current state of health.
We currently don’t utilise the time that patients are waiting to be seen by a specialist or the time that they are on the ESWL, waiting for their surgery. These two time periods can often add up to several years and will usually be a minimum of 6 – 8 weeks, even for the most urgent elective surgical procedures.
When a woman receives the news that she is pregnant, she is offered the opportunity to enrol in an ante-natal program. This consists of regular visits with many practitioners; GP and Specialist Obstetricians; midwives; ante-natal classes run by allied health practitioners and any other specialised investigations/treatments the woman requires to optimise her pregnancy and decrease risks.
A similar type of ‘program’, could be applied to a patient’s surgical journey, optimising not only their peri and post-surgical periods but also their pre-surgical care to decrease the risks associated with their procedure.
Optimised Pre-Surgical Care (OPSC) will therefore form a major body of work for the Statewide Surgical and Perioperative Care Network, aiming to improve patient outcomes and health care delivery. The Networks Steering Committee is currently evaluating any current programmes being used in this field and formulating innovative new ways to achieve an improvement in delivery of optimised pre-surgical care.
To read about more about the Network and its projects, see Statewide Surgical and Perioperative Care Clinical Network.
